|
When Alzheimer’s Meets Race,
Black Caregivers Face Toughest Challenges
By
Andrea Parrott, New America Media
May 30, 2012
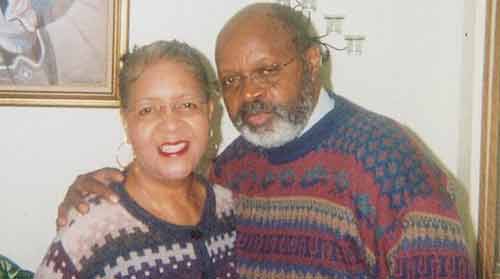
Juanita and
Chuck Williams
Picture
Credit: newamericamedia.org
Part
3 of a series. Click to read Part 1 and Part
2
MINNEAPOLIS, Minn.-- Juanita
Williams recalled when she was so tough she
was known as a “sheriff without a badge.”
For 20 years, she worked with mothers who
were dealing with substance abuse. When they
saw her coming to their homes, some of them
tried to run away. They knew she meant
business.
As a social worker for Hennepin
County, Williams did everything she could to
help pregnant women stay sober and others to
remain sober for their children’s sake.
Today, Williams focuses her energy
on the tender loving care she needs for her
husband of 40 years, Chuck Williams, 70. He
was diagnosed with early-onset Alzheimer’s
disease in 2003. She retired from her job in
July 2011. The emotional toll both of
working with the women and caring for her
husband had become too much to handle.
According to the Alzheimer
Association, African Americans in the United
States are two to three times more likely
than whites to be diagnosed with the
disease.
"Unbelievable"
Caregiver Stress
Family caregivers often experience
high levels of stress that can affect their
jobs and health, according to the
Alzheimer’s Association.
And Dorothea Harris, who runs
Family Memory Care for African Americans at
Volunteers of America in the Twin Cities,
said, “We have already lost a couple of
caregivers. They’ve died. The work is just
unbelievable.”
African American caregivers spend a
weekly average of 30 hours providing care
and are more likely to experience a higher
level of burden from caring for their loved
one, according to a recent Alzheimer’s
Association report.
Previously, Chuck had a successful
career as a University of
Minnesota-Extension recruiter and professor.
He participated in Toastmasters and could
give excellent impromptu speeches. Chuck was
a singer and writer who enjoyed his
community.
Now, Juanita oversees all of her
husband’s needs, including medication,
grooming, meals and activities.
It’s not easy, she explained: “He
puts his clothes on, and I’ll go in there
and help him because he has it on
backwards.--‘No, I’ll do it. I’ll do it,’
[he says], just like a kid learning how to
do that. I’ll sit there and let him do it.
And then sometimes he does it and sometimes
he doesn’t. So I just gauge in another time
when he’ll let me do it.”
As Juanita described part of her
day, she concluded, “It’s a lot of work.”
Care
at Home to the Breaking Point
Keeping Chuck at home for as long
as possible was a primary goal for Juanita,
and one key to doing so was enrolling him in
the adult day health care (ADHC) program at
the Wilder Foundation’s Community Center for
Aging in St. Paul three days a week. The
center offers dementia-specific programs for
elders who need that specialized attention.
The ADHC program gave Juanita
relief from caregiving and allowed her time
to complete errands. She felt less
comfortable having in-home respite care
services because she does not trust
unfamiliar people in her home. The program
has the more open environment that she
prefers.
According to Jocelyn Schowalter,
Wilder’s director of services in aging,
about half of those attending the ADHC
program are African American. Participants
can undergo testing to help families and
program staff learn what the person affected
with dementia can do in the program and at
home.
“The key is keeping that person
busy with meaningful activities,” Schowalter
said. Among the activities are physical
exercise, art, music, literature and
gardening.
Schowalter noted that among the
professional artists working with program
participants are dancers and drummers, as
well as a painter who does water painting, a
poet and a master gardener. Participants can
work in and enjoy the produce from the
garden located at the center.
Eventually, however, families may
face a time when the ADHC program or home
care are no longer appropriate options.
Juanita reached her breaking point
as Chuck reached the advanced stages of
Alzheimer’s. He could hardly speak any more,
walking became more difficult and he didn’t
feed himself.
“I couldn’t do it anymore,” Juanita
said. “He’s like a two-year-old.”
She allowed, “We had some good
years,” but Juanita found that now she
couldn’t leave Chuck alone for even a
moment. At night she constantly worried that
he would wander out of their apartment. Her
children assured her that she had kept their
father at home as long as possible.
“I hate this disease. I hate it,”
Juanita declared. “Our dreams, our goals
that we were going to do when we retire,
it’s gone,” she added.
Hardest
Option for Black Families
It was difficult for Williams to
consider assisted living or long-term care
as an option for her husband. In her family,
grandparents, aunts, and uncles received
care at home until they died.
“In the black family, you take care
of family members at home,” she said.
As caregiving for Chuck became more
difficult, though, Juanita began to consider
assisted living or a long-term care
facility. But she wondered where her husband
would receive adequate care.
“Not that anybody can do it [care
for her husband] better than me,” Juanita
asserted. “That’s not what I’m saying.
That’s why, wherever he goes, I will be
there, like any time.”
At the end of March of this year,
Chuck entered a memory-care unit at a
nursing home. “I go there every day,”
Juanita said. She conceded that she has had
difficulty adjusting to not having him at
home. She added, “The nursing home is no
picnic, and it’s the last resort.”
According to Harris of Family
Memory Care, distrust and the fear of
discrimination are key reasons why few
African Americans--only 19 percent according
to one study--consider long-term care
placement as an option.
She continued, “Because of the
stigma and because of the exploitation that
has taken place in the African American
community, there’s fear of the nursing
home.” She added, “We want to be sure that
our loved one is taken care of and who can
do that better than us.”
Distrust of long-term care homes
among African Americans is not unfounded.
Studies in recent years have shown that
disparities persist between homes serving
predominantly black and white residents. For
instance, a 2011 study in the Journal of the
American Medical Association showed patients
in homes with largely African American
clients get more bed sores.
Another study last year in Health
Affairs verified that black nursing home
patients are less likely than those in
mainly white facilities to receive flu
vaccinations. Still other research has
documented that African Americans in
long-term care tend to receive less pain
treatment and good end-of-life care.
Little
Cultural Competence
An additional concern for African
Americans in the Twin Cities is a lack of
cultural competence among staff in
facilities for rehabilitation, assisted
living or skilled nursing care.
According to the National
Institutes on Health, a culturally competent
health care system “acknowledges and
incorporates—at all levels—the importance of
culture… and adaptation of services to meet
culturally unique needs.”
For African Americans, for
instance, non-black staff should know that
black seniors might typically greet some one
they don’t know by saying, “Hi, Brother” or
“Hi, Sister,” and expect a friendly
response.
Overall, say experts, low levels of
culturally sensitive interaction, combined
with activities, resources and even facility
decorations that do not reflect cultural
diversity, can make nursing homes a lonely
place for minorities. Facility activities
directors should, for example, request that
local arts programs send African American
musicians and artists among those they
typically send. Or simply playing some
Motown tunes, not merely Doris Day or Frank
Sinatra could help brighten the day for
black residents.
For Juanita, prayer and input from
family eventually enabled her to feel that
she could make a positive decision to place
Chuck in a long-term care home.
She admitted, “I’m tired. I can’t
do it all like I use to—physically and
mentally and emotionally.”
Even Chuck noticed how weary she
seemed, Juanita said. He told her at one
point to rest. Juanita remembered his
concern: “He said, ‘You need to sit down
because you’re running. You’re doing too
much.’”
Juanita agreed: “I have not had a
breather,” she said, “I don’t get enough
time for me. It’s not about escaping--but I
can’t do it all. I cannot do it alone. It’s
hard.”
|



