back
|
 |
Health Disparities Among
Older Women:
By: Arlene S. Bierman
Journal of the American medical women's association, December 2001
Identifying
Opportunities to Improve Quality of Care and Functional Health Outcomes
Older women experience a high burden of chronic
illness, disability, and comorbidity, and this burden is highest among
socioeconomically disadvantaged and minority women. The consequences of a
mismatch between the organization, delivery, and financing of health care
for older women and their actual needs fall disproportionately on
low-income and minority women. New sources of data, such as the Medicare
Health Outcomes Survey, a new quality measure for Medicare+Choice
plans, will provide valuable information to practitioners about the health
and functioning of older women in general and about socioeconomically
disadvantaged and minority women in particular. This information can be
used to develop and implement interventions to improve the quality and
outcomes of care for vulnerable subgroups of older women. There is cause
for optimism that by improving the quality of clinical preventive services
and the management of common chronic conditions and geriatric syndromes it
will be possible to improve functional health outcomes, prevent or
postpone disability, and extend active life expectancy for all older women
while making progress toward eliminating health disparities among the most
disadvantaged. (JAMWA. 2001;56:155-159)
Reducing disparities in health and health care
associated with race, ethnicity, and socioeconomic position has emerged as
a major challenge for the United States health care system. These health
disparities persist into old age.
Gaining access to health care does not necessarily result in equivalent
treatment. Race, ethnicity, socioeconomic position, and other factors are frequently
associated with differential treatment. The proportion
of the population age 65 and older who are from racial or ethnic
minority groups is projected to grow from 16% in the year 2000 to 36% by
the year 2050 (16% Hispanic, 12% African American, 7% Asian and Pacific
Islander, and 0.6% Native American).
The aging of the "baby
boomers" and associated challenges for Medicare make it critical
that we address health care disparities among the increasingly ethnically
diverse older population, the majority of whom are women. Inequality of
care can no longer be viewed as the result of socioeconomic forces beyond
the control of clinicians and health care organizations.
The high burden of chronic illness, comorbidity, and disability among
older women, coupled with a health care system inadequately organized to
respond to these needs, makes addressing health disparities among older
women a pressing challenge.
Efforts to assess and improve quality of care for
older patients now include a specific focus on improving the management of
chronic illness and functional health outcomes,
which is of prime importance for older women.
Previous studies have examined how individual and community
characteristics, including use of services, are associated with older
women's health and functional status.
These studies have provided important insights into the epidemiology of
functional decline among older women. Few studies have examined the direct
impact of health care and policy on older women's health, and none have
addressed the interaction of health care and race, ethnicity, and
socioeconomic position on older women's ability to function. Evidence
suggests that improving the quality of clinical preventive services and
the management of chronic illness and common geriatric syndromes may have
a positive impact on functional health outcomes and form the foundation
for addressing disparities in health care among older Americans.
We focus here on how health care and the policies
that effect health care delivery can improve health outcomes and reduce health
disparities among older women. We present descriptive data
illustrating health disparities in older women from the Medicare Health
Outcomes Survey (MHOS), a new quality measure in HEDIS
2000, and provide selected examples of interventions that can improve
quality of care and reduce health disparities.
Two Conceptual Frameworks
We present 2 complementary conceptual frameworks that
clarify the relationships among the many factors that influence health
outcomes and help us to identify potential opportunities to improve care.
The first (Figure
1) illustrates the relationships among health policy; the organization
and financing of care; clinical practice; and the biological, individual,
social, and community factors that influence health outcomes.
It includes a patient-centered rather than disease-specific focus,
particularly relevant for older women (because many have multiple chronic
conditions). Patient-centered models recognize the net effect of
individual conditions and treatments on overall function in the context of
pyschosocial factors and patient values. Multiple domains of functioning,
including physical, emotional, cognitive, role, and social functioning,
contribute to overall health outcomes. A patient's functioning is
influenced by her biology (eg, genetics), individual characteristics (eg,
health beliefs and behaviors), family (eg, social support), and community
(eg, environmental factors, community services) as well as by her
interactions with the health care system. The clinician-patient
interaction is influenced by how the clinical setting is organized and by
the financial incentives created by payment mechanisms, which are in turn
influenced by health policy. All of the arrows in the framework are
bidirectional, reflecting the multiple, complex interrelationships that
influence health and function in older people.
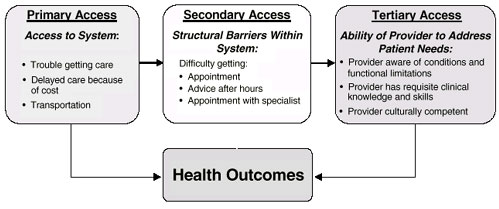
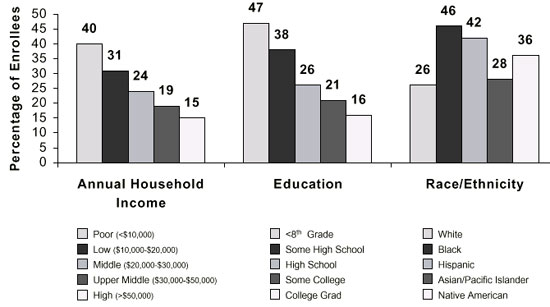
The second conceptual framework (Figure 2)
illustrates how access to and quality of care mediate health outcomes and
can help us identify opportunities for improving the interaction between
patients and providers. Primary, secondary, and tertiary barriers to
access must be addressed.
Primary barriers represent the first obstacle in getting care and include
such factors as lack of or inadequate health insurance, proximity of
providers, and lack of transportation. Secondary barriers are structural
barriers such as difficulty getting appointments, specialty referrals, or
advice after hours. Tertiary access reflects the ability of providers and
the health care system to understand and address the patient's needs,
including the provider's communication skills, cultural
competence, knowledge, and clinical skills. These barriers have a
disproportionate impact on low-income and minority
individuals
and on older people, especially those who are functionally impaired.
Health Disparities Among Older Women
A new measure of overall functional status required
for managed care plans that serve Medicare
beneficiaries is of particular relevance to efforts to improve functional
health outcomes and reduce health disparities among older women. The MHOS
is designed to measure change in self-reported function over 2 years.
Respondents are asked to provide information on symptoms, diagnoses, and
sociodemographic characteristics in addition to reporting on their ability
to function, assessed by the SF-36. The measure that will be reported for
health plans is the casemix-adjusted proportion of enrollees whose 2-year
change in function is worse compared to those whose function is the same
or better. Despite limitations of the survey, the large sample size of the
MHOS affords an unprecedented opportunity to understand the health and
functional status of low-income and minority elderly women and to examine
how race, ethnicity, income, and education affect quality and outcomes of
care. These data will be used at the federal, state, and health plan
levels to design and evaluate interventions aimed at improving functional
health outcomes for Medicare
managed care enrollees. Descriptive data from the 1999 baseline survey
of 91 314 community-dwelling women age 65 and older illustrate existing
health disparities.
The second conceptual framework (Figure
2) illustrates how access to and quality of care mediate health
outcomes and can help us identify opportunities for improving the
interaction between patients and providers. Primary, secondary, and
tertiary barriers to access must be addressed.
Primary barriers represent the first obstacle in getting care and include
such factors as lack of or inadequate health insurance, proximity of
providers, and lack of transportation. Secondary barriers are structural
barriers such as difficulty getting appointments, specialty referrals, or
advice after hours. Tertiary access reflects the ability of providers and
the health care system to understand and address the patient's needs,
including the provider's communication skills, cultural competence,
knowledge, and clinical skills. These barriers have a disproportionate
impact on low-income and minority individuals[7]
and on older people, especially those who are functionally impaired.
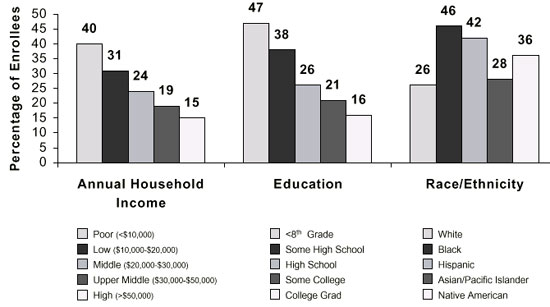
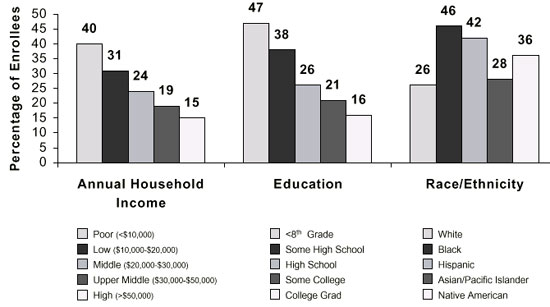
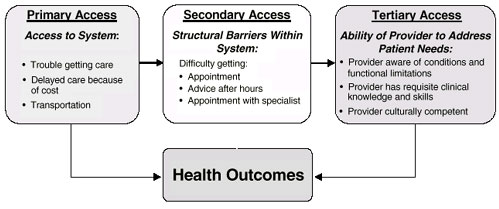
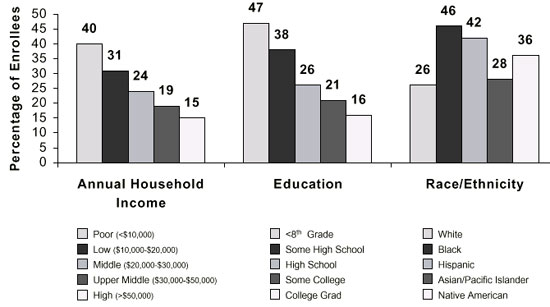
Differences in Socioeconomic Position.
There are large differences in income, education, and
marital status among racial and ethnic groups of older women that can
influence effective access to care (Figure
3). Twenty percent of all women age 65 and older enrolled in Medicare
managed care reported annual household incomes of less than $10,000, and
income varied markedly by race and ethnicity. African-American, Latina,
and Native American older women were significantly more likely to be
living in poverty than non-Hispanic white and Asian older women.
Out-of-pocket health care costs place considerable financial strain on
low-income beneficiaries.
One study found that the 60% of beneficiaries with incomes below the
poverty level who did not receive Medicaid spent half their incomes, on
average, on out-of-pocket expenses, whether they were enrolled in Medicare
managed care or in the traditional
fee-for-service program.
Many women had not benefited from formal education,
placing them at risk for low health literacy.
Thirty-one percent of all women age 65 and older enrolled in Medicare
managed care had not graduated from high school, 12% of whom had less than
an eighth-grade education. At least half of all African-American, Latina,
and Native American women reported less than a high school education (Figure
3).
Older women are being called on to make increasingly complex decisions
about Medicare coverage, to choose among a growing array of therapeutic
interventions, and to become active participants in their care. Their
ability to do this effectively will depend on having information
communicated clearly in a manner that takes literacy level into account.
Older women were more likely than men to live alone,
and when they lived with others, they were more likely to be caregivers
for spouses or grandchildren. Caregiving responsibilities and resulting
competing demands can result in barriers to care. Figure 3 shows racial
and ethnic differences in marital status. African-American women were more
likely to be unmarried; they were also more likely to live with other
relatives, so that about 40% of white and African-American women lived
alone. Hispanic and Asian women were least likely to live alone.
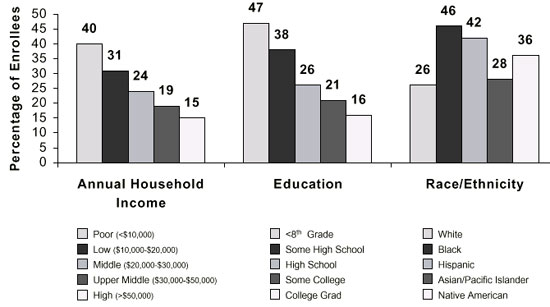
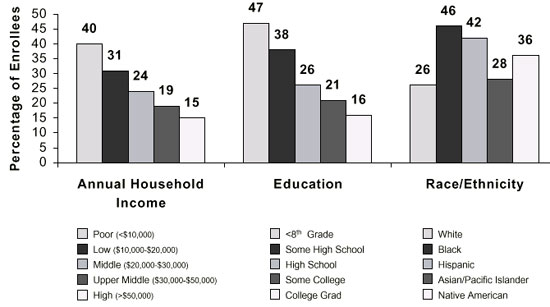
Differences in Global Health.
Global health is highly correlated with income
and education. Figure
4 shows differences in the proportion of women in the MHOS who
reported fair or poor health by income, education, and ethnicity. After
adjusting for age, the lower a woman's income, the more likely she was to
report fair or poor health. Women reporting annual household incomes of
less than $10,000 were more than twice as likely to report fair or poor
health as were women reporting annual household incomes of more than
$50,000. Nearly one-half of respondents with an eighth-grade education or
less reported that they were in fair or poor health. These women were
nearly 3 times more likely to report that they were in fair or poor health
than were college graduates,
highlighting the paradox that women with the fewest resources to negotiate
the health care system have the highest burden of illness.
Chronic Conditions and Symptom Severity.
The proportions of women who reported chronic
conditions are shown in the table. More than half of the women in the
survey reported hypertension
or arthritis,
and one-third reported cardiovascular
disease or symptoms of urinary incontinence. Fifty-two percent of women reported 3 or more chronic
conditions. Women with low incomes and less education were significantly
more likely to report each of these conditions. Prevalence of chronic
illness varied by race and ethnicity, with African-American and Native
American women reporting the highest burden of illness.
Low-income and less educated women were not only more
likely to report chronic illness, but they were also more likely to report
symptoms. For example, 58% of poor women reported having arthritis, and
54% of poor women with arthritis reported moderate or severe pain much of
the time. Fifty-one percent of women with annual household incomes of
$50,000 or more reported arthritis, 37% of whom reported having moderate
or severe pain much of the time. A similar pattern by income was seen
among women reporting ischemic
heart disease and chest pain with exercise all or most of the time.
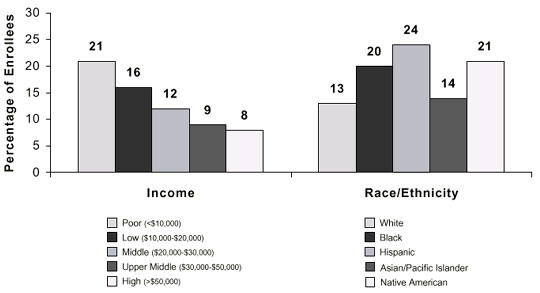
Differences in Depressed Mood.
The proportion of older women reporting depressed
mood differed by income and race/ethnicity (Figure
5). Low-income women were much more likely to report that they felt
depressed or sad much of the time in the past year than were their more
affluent counterparts. Twenty-one percent of women who reported an annual
income of less than $10,000 indicated that they felt depressed or sad much
of the time in the past year compared to 8% of women with annual household
incomes of more than $50,000. Nearly 1 in 4 Latina women reported
depressed mood. African-American and Native American women were more
likely to report depressed mood than were white and Asian women.
Depression often goes undiagnosed, and screening for depression coupled
with interventions to improve its management has been shown to improve
quality of care for depression in primary care practice.
Differences in Comorbidity and Disability.
Comorbidity and disability are common problems in
older women.
Women who had low incomes, who had less than a high school education, or
who were African American were more likely to report 3 or more chronic
conditions or limitations in activities of daily living (ADLs). A prior
study using the 1992 Medicare
Current Beneficiary Survey found that women age 65 and older with less
than a high school education were nearly twice as likely to report 3 or
more chronic conditions or ADL limitations as women who had more than 12
years of education.
Although it is a major concern for older patients, many doctors do not
routinely assess their functional
status.
A survey of individuals age 80 and older in New England found that many
perceived that their physicians were unaware of their marked functional
impairments, including physical limitations,
moderate to severe pain, and impairments due to mental health.
Targeting Critical Gaps
By systematically and strategically targeting
critical gaps in the organization, delivery, and financing of care for
older women, we can make progress toward eliminating the large
socioeconomic and racial/ethnic disparities in health described above.
These gaps can be categorized into 5 key areas: access, quality,
organizational, evidence, and payment gaps. Clinicians can play a central
role in improving care for older women, but cannot do it alone. Systemwide
changes will be required. Below we provide examples of approaches that may
be used to narrow gaps in these areas.
Access Gaps
Providers can increase access for their patients by
identifying and targeting primary, secondary, and tertiary barriers within
their practices. Providing patients with information about such federal
programs as the Medicare
Buy-In Qualified Medicare Beneficiaries can reduce financial
barriers. Many states sponsor pharmacy benefit programs for the low-income
elderly that can help older women purchase needed medications. Small
organizational changes at the practice level, such as facilitating
scheduling of urgent appointments or developing efficient mechanisms to
address patient concerns by telephone, may help reduce secondary barriers.
Attention to such issues as cultural competence and health literacy can
serve to reduce tertiary barriers to care.
Quality Gaps
In recent years much attention has been focused on
the failure of our health system to consistently provide high-quality
care. The Institute of Medicine's report Crossing
the Quality Chasm emphasizes gaps in the quality of care for
chronic conditions and describes strategies to help close these gaps.
Closing the quality gap for older women will require improvement across
the continuum of care, including health promotion, clinical preventive
services, management of chronic illness, coordination and accountability
across different sites and settings of care, and coordination between
clinical and community services. Clinical interventions can reduce the
risk of both acute events such as stroke and hip fractures and the
progressive loss of function from such conditions as arthritis and
congestive heart failure. As the population ages, it will be increasingly
important for basic geriatric principles to be incorporated into practice.
Organizational Gaps
Health system redesign is needed to close
organizational gaps that present obstacles to improving the care of
chronic illness. Wagner et al
have developed a chronic
care model that provides a framework for systems change that has been
used to improve the quality of care in diverse settings. This model
recognizes the critical role of the patient as an active participant in
her care and the value of self-management interventions. Clinical
leadership is a key element needed in this model.
Evidence Gaps
Gaps exist in our knowledge of how best to organize,
finance, and deliver health care services that will improve the functional
status of older women; of the most cost-effective ways of achieving these
improvements; and of how to implement existing knowledge of what improves
function in clinical practice. Evidence on how best to take into account
the impact of multiple comorbid conditions on clinical decision making is
needed. Outcomes and effectiveness research can provide the evidence to
close some of these gaps.
Payment Gaps
Although this paper has focused on health status,
much work needs to be done to develop payment mechanisms that align
financial incentives with the provision of high-quality, comprehensive,
coordinated care for older women (Figure
1). Shortcomings in the reimbursement of care for chronic illness and
disability present a barrier to innovations to improve the quality of care
for older women. For example, traditional fee-for service Medicare rewards
the acute care model and creates incentives for overuse of services, but
not for prevention, and does not allow for financing of innovative models
of care for chronic illness. Feedback from providers about the resources
needed to improve functional health outcomes could provide valuable
information to inform payment policy.
Conclusion
Enormous opportunities exist to improve the health of
and health care for older women and to benefit socioeconomically
disadvantaged women, who experience the highest illness burden and are
disproportionately affected by the shortcomings of our health care system.
Enhancing our understanding of factors that contribute to racial/ethnic
and age disparities in quality of care will allow us to strategically
target and eliminate them. New sources of data such as the MHOS will
provide valuable information about the health and functioning of older
women that can be used to develop, implement, and evaluate interventions
aimed at improving quality and outcomes of care for low-income and
minority women. Improving the quality of clinical preventive services and
the management of common chronic conditions and geriatric syndromes will
make it possible to improve functional health outcomes, prevent or
postpone disability, and extend active life expectancy for all older women
and to make progress toward eliminating health disparities among the most
disadvantaged.
We acknowledge Samuel C. Haffer, PhD, and Yi-Ting
Hwang, PhD, for their contributions to the analysis of the MHOS data.
Table 1.
Self-Reported Chronic Disease and Symptom Prevalence of Women Age 65 and
Older in Medicare Managed Care,* %
|
Chronic Disease Prevalence
|
|
|
|
High blood pressure
|
|
56.4
|
|
Arthritis
|
|
55.4
|
|
Arthritis pain
moderate/severe
|
|
49.3
|
|
Cardiovascular disease†
|
|
34.5
|
|
Ischemic heart
disease
|
|
15.1
|
|
Stroke
|
|
7.4
|
|
Congestive heart
failure
|
|
6.4
|
|
Other heart
condition
|
|
20.7
|
|
Sciatica
|
|
23.4
|
|
Diabetes
|
|
15.4
|
|
Asthma/COPD
|
|
12.4
|
|
Cancer
|
|
12.8
|
|
Inflammatory bowel disease
|
|
6.0
|
|
Symptoms
|
|
|
|
Difficulty
controlling urination
|
|
30.6
|
|
Felt depressed or
sad‡
|
|
14.5
|
|
Back pain§
|
|
12.7
|
|
Shortness of
breath||
|
|
10.4
|
|
Chest pain with
exercise
|
|
3.0
|
|
Sensory Impairment
|
|
|
|
Difficulty hearing
|
|
10.7
|
|
Difficulty seeing
|
|
6.4
|
|
Comorbidity
|
|
|
|
3 or more chronic conditions
|
|
51.5
|
|
Mean no. comorbid conditions (SE)
|
|
2.9 (0.01)
|
|
*Based on the responses of 91 314 community-dwelling women age 65
and older responding to the 1999 MHOS Cohort 2.
†Reports at least one of the following conditions: ischemic heart
disease, stroke, congestive heart failure, other heart condition.
‡Felt sad or depressed much of the time in the past year.
§Low back pain interferes with usual daily activities all or most
of the time.
||Shortness of breath all or most of the time when walking less than
1 block. All/most of the time.
|
|
|
Figure 1.
Policy, organization, finance, clinical practice, patient factors, and
functional health outcomes.
Figure 2.
Access, quality, and health outcomes.
Figure 3.
Income, education, and marital status of wonen age 65 and older enrolled
in Medicare managed care by race/ethnicity.
Source: 1999 Medicare Health Outcomes Survey Cohort 2 Baseline Data.
Figure 4.
Proportion of women age 65 and older enrolled in Medicare managed care
reporting fair or poor health by income, education, and race/ethnicity.
Source: 1999 Medicare Health Outcomes Survey Cohort 2 Baseline Data.
Figure 5.
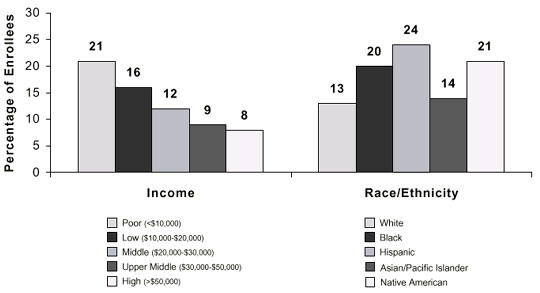
Proportion of women age 65 and older reporting depressed mood by income
and race/ethnicity.
Source: 1999 Medicare Health Outcomes Survey Cohort 2 Baseline Data.
|